- Written by SSI VA
- On Apr 03 2014,
- In General surgery
Total Knee Replacement
Total knee replacement is recommended for patients suffering from Arthritis, extreme pain and limited function.
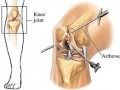
To understand knee replacement surgery it is important to understand how your knee works. Your knee joint works like a hinge at the junction of two bones, the thigh bone and the shin bone. The ends of the bones are covered with a thick layer of soft, white cartilage. If this cartilage is damaged or worn away, the underlying bones rub together, causing pain and lack of mobility.
Total knee replacement will help an individual return to their personal independence, often pain free. It may also straighten the leg; improve stability and the function of the joint. In a total knee replacement, the surface of the joint is replaced with metal and plastic surfaces which can function similar to normal joint. This is accomplished by surgically trimming the ends of the bones and replacing them with new metal and plastic surfaces. Essentially, a total knee replacement is a “resurfacing” of the joint. Most of the ligaments, tendons and muscles around the knee joint are retained. The new joint’s surfaces mimic the natural knee it replaces.
Before a total knee replacement surgery you will need the following:
- You will need a thorough dental examination to ensure you do not have any dental problems and infections which could travel through your bloodstream and infect your hip replacement. Any infection needs to be treated before your surgery.
- You will need an examination by an internist to specify any medical problems you may have that could interfere with your total knee replacement.
Your doctor will schedule a preadmission evaluation which may include some or all of the following.
- Medical history
- Anesthesia interview
- Blood and urine tests
- Electrocardiogram
- X-rays
During the first six weeks after surgery, while the muscles and tissues around your knee are healing, you will need to follow certain activity restrictions. To help you during your recovery SSI can arrange the following.
- A bi lingual nurse
- A physical therapist
- An apartment/house/hotel with easy access, dvd player and a large selection of movies
- Cleaning and laundry services
- Food shopping and preparation
- Massage therapists
- Tours of the island }
Joint replacement procedures (also called arthroplasties) are done when a patient experiences severe, incapacitating hip pain due to osteoarthritis, rheumatoid arthritis or injury. The old joint is replaced with a new mechanical joint called a prosthesis.
The knee is a hinge joint where the large bone in your lower leg (or tibia) connects with the end of the thigh bone or femur. A healthy knee has smooth cartilage that covers both the end of the tibia and the end of the femur. The smooth cartilage allows the two bones to glide together when you bend your knee. Your knee joint is surrounded by muscles and ligaments to support your weight and allow your joint to work smoothly.
Severe pain and decreased movement can result as the cushion of cartilage wears away in a knee joint affected by osteoarthritis or other diseases. The joint bones rub against each other, becoming rough, pitted and irritated.
A knee prosthesis is comprised of smooth surfaces, much like a healthy knee. The femoral component caps the end of the thigh bone; the tibial component covers the underside of the knee joint surfaces and allows you to move and walk easily without pain.
What are the risks involved in having a total knee replacement?
We want you to understand the benefits and risks of knee replacement surgery. The ultimate goal is for you to regain function of your knee with minimal pain and discomfort. Most people recover smoothly from surgery. However, complications are possible. These occurrences are rare and are almost always treatable.
Complications you should be aware of:
Blood clots may occur when blood flow is slowed due to the break in activity you will experience after your surgery. The following measures are helpful in preventing this condition:
- Ankle pump exercises after surgery
- Elastic stockings or foot pumps to improve circulation
- Elastic stockings or foot pumps to improve circulation
- Medication to thin your blood
- Getting out of bed several times each day starting either the day of surgery or the next day
Even with the best of care, it is still possible for blood clots to form. It is important that you watch for any signs of blood clots and let medical staff know immediately if you experience any of the symptoms listed below:
- Swelling
- Redness
- Pain
- Tenderness and warmth in the calf or lower leg
Infection is a possibility with any surgery.
- With joint replacement surgery, infection may be at the incision (the surface) or inside your body around your prosthesis. To help prevent infections, you will be given IV antibiotics after surgery.
- It is also possible to get an infection at home, after you leave the hospital. Again, antibiotics generally take care of these types of infections, but in rare cases, additional surgery may be needed to remove an infected prosthesis for replacement with a new one.
Dental Injury
- Teeth may become chipped, loosened or dislodged during your surgery and recovery period. Please let your anesthesia team know of any dental problems you may have.
Reactions to anesthesia or pain medication are other types
of complications that can occur.
- Please let your doctor or anesthesiologist know if you have ever experienced a reaction during a previous surgery.
Nerves close to the joint replacement may be damaged.
- Over time, these nerves may improve, or completely recover.
Knee prosthesis loosening
- Many years after your joint replacement, your prosthetic knee may become loose. Surgery may need to be performed to revise the joint replacement.
Knee Prosthetic wear
- Some wear is common on all joint replacements. Surgery may be needed to revise the joint replacement when the wear is severe. The lifetime of your knee replacement should be between 13 and 15 years.
Knee Prosthetic breakage
- While very rare, the metal or plastic joint in a replacement may break. Again, surgery would be required to revise the joint if this occurs.
Blood donors are routinely screened for:
- Blood type
- Infections
- HIV (the AIDS virus)
- Hepatitis B and C: an infection of the liver and the blood
- Syphilis: a sexually transmitted disease that is also carried by blood
- HTLV: a virus that causes certain infection
Other possible risks include:
- Fever
- Chills
- Rash, itching or hives
- Infection
A Positive Approach
Preparing mentally for your knee replacement surgeryis just as important for you and your family or support person as it is for your surgeon and the rest of the medical team involved in your knee replacement procedure. Because of medical advancements, total joint replacement surgery is possible to relieve your pain and discomfort and improve your activity level.
It is important to remember that the pain and activity limitations after knee replacement surgery will be different than what you are experiencing now, and they will be short term. A significant portion of the recovery process is using your new joint by walking and doing the exercises that your doctor orders.
Depending on your condition, your recovery and exercise plan will be tailored to meet your needs. Each patient recovers differently and joint replacement revisions often progress at a slower pace than the initial surgery.
Your stay in the hospital will be short and your recovery will be continued after discharge in your home, with family, or at an extended care – rehab center. It is important for you to make a commitment to follow your doctor’s instructions and work on your exercise plan after surgery in order to benefit most from the joint replacement. If you or your family need support, either physically or emotionally, coping with surgery and recovery, please talk with the staff.
*The improved lifestyle after recovery is worth the risk and stress of surgery!
The family’s role in your recovery
Your family and friends are very important in helping you during your recovery after your knee replacement surgery. They can help:
- Stock up on canned and frozen or packaged food
- Your family and friends are very important in helping you during your recovery. They can help:
- Stock up on canned and frozen or packaged food
- Move food to cabinets between your waist and shoulder level, helping you avoid reaching and bending
- Prepare a room with all the needed supplies so that you can rest during the day
- Remove rugs and other clutter for safe walking
- Run errands, grocery shop, and drive you to follow-up doctor’s appointments
- Arrange for needed equipment
*Surgery is your primary path toward getting yourself back to being the person you want to be , so don’t let any unnecessary delays stand in your way!
Going Home after Knee Replacement
Discharge instructions
- You will be given written discharge instructionsand prescriptions for any medications needed after discharge.
- We will go over these instructions with you. If there is any information that you do not understand, please ask the staff before you leave.
Recovery
- The past few weeks you have prepared for your knee replacement surgery, waited to enter the hospital, undergone surgery, learned to walk with your new joint, and made plans for going home.
- You are stable enough to be discharged from the hospital. For the next six to eight weeks, you will continue to heal and recover from surgery. You should balance periods of activity with periods of rest.
- Do not try to overdo or push yourself to the point of pain or exhaustion.
Medication
- Resume medications that you were taking before surgery unless instructed otherwise by your doctor.
- You will be given a prescription for pain medication.
As your pain decreases, you may take Tylenol . - Your doctor may prescribe medication to prevent blood clots from forming, such as aspirin or Warfarin (Coumadin).
- If you are on Warfarin, it is important to closely follow instructions that your nurse or doctor gives to you.
Activity
- Follow the activity guidelines and exercises as instructed by your doctor or physical therapist.
Hip precautions:
- Limit sitting to 30 – 45 minutes at a time.
- Use your walker or crutches. You may also be instructed to wear a special knee brace which can be removed when sitting or lying in bed.
- Watch for signs of infection and swelling.
- We recommend limiting stairs to one flight up and down per day.
- Use your adaptive equipment and do your exercises to regain strength and function!
Walking
- Use your walker or crutches for each step when walking. Progress to use of a cane when directed by your therapist or physician. You may feel that you can walk without an aid, but the bones take six to eight weeks to heal.
- Walk daily for increasing distances, allowing for rests between activities.
Sitting
- Do not sit longer than 30 minutes at a time. Get up, walk, and change positions.
- On long car trips, stop at 30 minute intervals. Get out and move around.
- With lack of movement, your knee may become stiff, swollen, and you are more prone to blood clots.
- Use a pillow or chair cushion on all low chairs.
- Use a raised toilet seat if instructed to do so.
- Do not rest in recliners. The reclining position does not aide circulation or reduce swelling.
Stairs
- If you need to use stairs, we recommend making only one trip up and down each day. Be careful and hold onto the railing or another person for support when using the stairs.
Sports
- Do not participate in sports during the first three months after your knee replacement surgery.
- Do not use exercise equipment, whirlpools or spas until your doctor tells you it is okay. Please talk with your doctor about the type of sports you like to do.
- You may eventually resume some sports that do not put your knee at risk, such as golfing, swimming, bicycling and dancing.
Sexual activity
After knee replacement surgery, many people are worried about resuming sexual activity. In reality, the pain and stiffness associated with your bad knee before surgery probably already interfered with intercourse.
Since your surgery will help decrease most of that discomfort, you may now be more comfortable during sexual activity. You may resume sexual activities as soon as you feel able.
Water beds
- If you have a water bed, tell your physical therapist.
Driving
- Do not drive until your doctor tells you it is okay.
Care of your wound
- If your wound was closed with staples,arrangements will be made to remove the staples that hold your incision together.
- Wash your incision gently with soap and water and pat it dry.
- You may shower if you have a walk-in shower.
- Do not take a bath.
- Do not use lotions on your incision until your doctor okays it.
Signs of infection
Each day with your bath/shower, look at your incision for the following signs of infection:
- Redness
- Swelling
- Drainage
- If you notice any of these signs, call your doctor immediately.
Antibiotics
- An infection in another part of your body (lungs, kidneys, mouth, skin, etc.) could possibly spread to your new joint.
- Contact your family doctor and orthopaedic
surgeon with any type of infection. - To protect your joint you may need to take antibiotics before certain procedures, such as dental care or a surgical procedure.
Swelling
- Swelling (also called edema) is common after surgery. Swelling may or maynot occur in the hospital or after you are home and more active.
- The most common areas for swelling are the foot, ankle, knee, and at times, the thigh.
- To decrease swelling, lie with your operative leg elevated so that your foot is higher than your heart. This can be done during your rest periods for at least 45 minutes, 2-3 times during the day. Also, place a cold pack on the affected area for 20 to 30 minutes.
Compression stocking (if ordered)
- Wear your white compression hose during the day for two weeks.
- Wear them as much as possible, especially during the day.
- Compression hose should be removed at night as they can cause pressure sores on heels.
Follow-up
- If staples were used to close your incision, an appointment for staple removal will be made for you prior to discharge.
- You will need to contact your surgeon’s office to schedule a six-week follow-up appointment.
by SSI VA
Categories
Recent Posts
-

Dental Implants
Dec, 30, 2015
-
General Dental Crowns
Dec, 30, 2015
-
Terms & Conditions
May, 26, 2015
-
Payment & Privacy Terms
May, 26, 2015
-
Dental Surgery
May, 26, 2015
-
Orthopedic & General Surgery:
May, 26, 2015
-
Eye Surgery
May, 26, 2015
-
Plastic Surgery:
May, 26, 2015
-
Site Map
May, 26, 2015
-
Links
May, 26, 2015










Leave a Comment