- Written by SSI VA
- On Mar 26 2014,
- In Eye surgery
LASIK Wavefront: Laser Eye Surgery
LASIK eye surgery is a laser eye surgery that is pretty cheap nowadays and is a life changing experience. Imagine never having to find your glasses AGAIN, or struggle with putting in your contacts. There is nothing like being able to just wake up and see!!
Patients with near-sightedness, far sightedness and astigmatism can now reduce or eliminate their dependence on contact lenses and eyeglasses through LASIK (laser assisted in situ keratomileusi). South America many people are surprised to hear has always been at the forefront of technology for eye surgery. 30 years ago refractive surgery was first developed in South America and as a result the most experienced doctors in the world, who not only use the latest technology but actually help develop it, are there.
The newest innovation to LASIK is a diagnostic device known as Wavefront. Wavefront is an extremely accurate device that maps any imperfections of your cornea and as a result there is less scar tissue and an increased probability of seeing 20/40 or better. It also allows people previously denied LASIK, due to thin corneal walls, the opportunity to undergo this life changing treatment.
ARE YOU A CANDIDATE FOR LASIK?
Here is a quick checklist to see if you are a good candidate for LASIK eye surgery? Every individual is different and nothing can replace a thorough examination by your optometrist to qualify you as a candidate.
- Are you 18 years or older?
- Has your prescription stayed the same or had only a minor change within the last year?
- Do you have a moderate prescription for myopia (near sightedness) or hyperopia (far sightedness)?
- You have never had eye surgery before? ( e.g. cataract, glaucoma,)
- Do you currently have cataracts? Or Glaucoma?
- Do you have a medical condition which may interfere with the healing process?
- Autoimmune or immunodeficiency
- Uncontrolled diabetes
- Degenerative disease of the cornea
- Cancer
- Lupus
- Rheumatoid arthritis
- Are you currently using any of the following drugs such as isotretinoin (Accutane 2 ) for acne treatment or amiodarone hydrochloride (Cordarone 3 ) for normalizing heart rhythm.
- Do you have severely dry eyes?
- Are you pregnant or nursing?
If you answered yes to questions 1-3 and NO to questions 4-9 you may be a good candidate for LASIK. Before you travel to receive LASIK it is very important that you visit your local optometrist and confirm your candidacy.
1-. Explanation of the procedure
LASIK is a form of outpatient corneal surgery in which, under local anesthesia, a surgeon uses a specialized and precise flap-making instrument, called a microkeratome, to create a thin flap of corneal tissue. This flap is raised and laid back while still attached to the cornea. The surgeon then uses an excimer laser to remove a pre-determined amount of corneal tissue from the exposed bed of the cornea. The amount of tissue to be removed is calculated based on the pre-operative determination of the power of your eye. The flap is replaced and within minutes natural forces hold the flap down on the cornea. Usually, within a few hours, the surface epithelium (“skin”) of the cornea begins to grow over the cut edge of the flap to seal it into position. LASIK can be used to correct nearsightedness (myopia), farsightedness (hyperopia), and astigmatism.
2-. Understanding How Your Eye Works
In order to decide whether to undergo the Procedure, it is helpful to understand how the eye works. The eye is like a camera. The cornea is the clear, dome-shaped window that forms the front wall of the eye. The retina is the light-sensitive tissue in the back of the eye that connects to the brain. The retina acts like the film in a camera. The cornea at the front of the eye acts as a lens that focuses light onto the retina, producing an image on the retina that gets transmitted to the brain and interpreted as vision. The curve of the cornea determines the power of the corneal lens and whether the incoming light rays from distant objects focus directly onto the retina. When light does not focus directly on the retina, the eye has a refractive error. This means that with the appropriate “refractive correction” lenses, incoming light rays become focused onto the retina, producing clear vision.
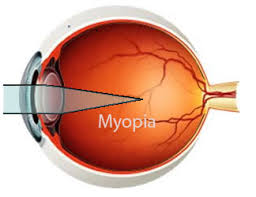
- Myopia/Nearsightedness
In the normal eye, the cornea focuses light rays directly on the retina, resulting in clear vision
without glasses or contact lenses. In myopia , or nearsightedness , the eye is longer than
normal. The light rays come together at a point in front of the retina, and are out of focus on
the retina. Distant objects are blurred, while nearby objects can be clear.
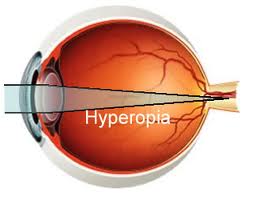
- Hyperopia/Farsightedness
In hyperopia, or farsightedness , the eye is shorter than normal. The light rays come together
at a point behind the retina, and are therefore out of focus on the retina. Nearby objects can
appear blurry, while distant objects are clearer. Very farsighted patients will report that even
distant objects appear blurry.
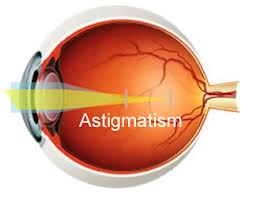
- Astigmatism
In the normal eye, the cornea is curved the same in the horizontal and vertical directions, like
a baseball. When the light rays hit the cornea, they focus at a single point. In astigmatism ,
the curve of the cornea is not the same in the horizontal and vertical directions. The cornea
looks like a football, with a steep curve on one side and a flat surface on the other.
As a result, light rays entering the cornea do not focus at a single point, causing distorted
vision. Many people with myopia or hyperopia have some degree of astigmatism.
In all of these conditions, the person needs some type of corrective lens, such as glasses
or contact lenses to focus the light properly. LASIK is used to change the shape and curve
of the cornea in order to correct myopia, Hyperopia and astigmatism.
3-. WAVEFRONT-GUIDED TREATMENT –What is it?
As technology advances, additional treatment options become available to patients. One such procedure is wavefront treatment (also referred to as “custom ablation” or “custom treatment”).
Eyeglasses and contact lenses address what’s known as ‘low-order aberrations’, of which nearsightedness, farsightedness, and astigmatism are symptoms.
Wavefront treatment corrects additional visual imperfections called ‘high-order aberrations’ (e.g., halos, spikes, starbursts, some night vision problems, etc.), improving visual acuity and visual quality beyond that which is possible with eyeglasses or contact lenses, or other, less evolved laser eye treatments. These high-order aberrations are mapped, and a customized laser treatment plan is developed to correct them.
Wavefront treatment involves creating a sophisticated corneal map of the eye and then combining that with an analysis of the visual system of the eye using a Wavefront analyzer, or aberrometer, which studies the way the eye bends light rays, improving visual quality potential. A precise measurement of all the aberrations of the eye provides a broader treatment range and allows patients to be treated that might have otherwise been ineligible. The entire visual system is analyzed, from the corneal surface through the crystalline lens of the eye, all the way to the retina, which is at the back of the eye. This combined analysis is then applied directly to the cornea via laser treatment.
These steps represent a far more detailed assessment and treatment of the visual system than available previously, whereby visual imperfections are virtually eliminated. Wavefront treatment can be done in conjunction with either LASIK or PRK, allowing one the opportunity to potentially see 20/20 or even better.
4-. Chances of Success
Chances of Success in LASIK
|
Myopia, Myopia with Astigmatism |
Chances of seeing 20/40* or better after LASIK |
| Low myopia (-6 or lower) |
99% |
| Moderate myopia ( between -6 and -10) |
97% |
| High myopia (-10 or higher) |
85% |
|
Hyperopia, Hyperopia with Astigmatism |
Chances of seeing 20/40* or better after LASIK |
| Low hyperopia (+4 or lower) |
99% |
Chances of Success in LASIK of IUMO.
|
Myopia, Myopia with Astigmatism |
Chances of seeing 20/40* or better after LASIK |
| Low myopia (-6 or lower) |
99.8% |
| Moderate myopia ( between -6 and -10) |
99.3% |
| High myopia (-10 or higher) |
96% |
|
Hyperopia, Hyperopia with Astigmatism |
Chances of seeing 20/40* or better after LASIK |
| Low hyperopia (+4 or lower) |
100% |
*A visual acuity of 20/40 of better is required to pass the driver’s license examination. It is therefore considered the legal “normal” visual acuity.
5-. The Process
First step initial exam
If you wear contact lenses, it is a good idea to stop wearing them before your baseline evaluation and switch to wearing your glasses full-time. Contact lenses change the shape of your cornea for up to several weeks after you have stopped using them depending on the type of contact lenses you wear. Not leaving your contact lenses out long enough for your cornea to assume its natural shape before your and exam and surgery can have negative consequences. These consequences include inaccurate measurements and a poor surgical plan, resulting in poor vision after surgery. These measurements, which determine how much corneal tissue to remove, may need to be repeated at least a week after your initial evaluation and before surgery to make sure your measurements have not changed.
You should tell your doctor about your past and present medical and eye conditions and any medications you are taking including over the counter medications and any allergies you may have. You should have the opportunity to ask your doctor questions during this discussion.
Your doctor should perform a thorough eye exam and discuss whether you are a good candidate for Lasik and what the risks, benefits and the alternatives of the surgery are. You should know what to expect before, during and after the surgery and what your responsibilities are. Give yourself plenty of time to think about the risk/benefit discussion, to review any informational literature provided by your doctor, and to have any additional questions answered by your doctor before deciding to go through with surgery and before signing the informed consent form.
Second Step (Pre- procedure)
Contact Lenses
Contact lenses can “warp” the corneal surface, which changes the corneal curvature and leads to a measurement of your refraction that is not representative of your true refraction. In order to properly calculate the treatment to correct your refractive error, you will have to stop wearing contact lenses at some stage prior to surgery. The time interval that you must go without wearing contact lenses depends on the type of lens that you use and the length of time you have used them.
- Soft contact lenses may not be worn for at least one (1) week prior to the pre-operative exam. Soft contact lenses may not be worn for at least one (1) week prior to the Procedure.
- Soft toric lenses may not be worn for at least one (1) week prior to the pre-operative exam. Soft toric lenses may not be worn for at least one (1) week prior to the Procedure.
- Gas permeable lenses may not be worn for at least four (4) weeks prior to the pre-operative exam (or 8 weeks if you have worn them for more than 20 years or 12 weeks if you have worn them for more than 30 years). Gas permeable lenses may not be worn for at least six (6) weeks prior to the Procedure.
- True hard lenses (PMMA) may not be worn for at least twelve (12) weeks prior to the pre-operative exam. True hard lenses (PMMA) may not be worn for at least twelve (12) weeks prior to the Procedure.
Exceptions to the above rules exist and you can discuss these with your eye physician.
Your doctor will order blood tests to be performed.
Day before surgery and day of surgery
You should stop using:
- Creams or lotions
- Make-up
- Perfumes
- Hair products that contain alcohol such at hair spray or mousse
These products as well as debris along the eyelashes may increase the risk of infection during and after surgery. Your doctor may ask you to scrub your eyelashes for a period of time before surgery to get rid of residues and debris along the lashes.
Make sure you bring with you a pair of sunglasses, your eyes will be sensitive and irritated by light for the first 24 to 48 hours.
Avoid alcohol 24 hours prior to and 48 hours after your surgery, as this tends to dehydrate the tissues.
Wear comfortable clothing on your surgery day. Avoid clothing such as wool that may generate lint in the surgical suite. Wear minimal jewelry and bring only necessary personal items.
Before your surgery
You will be instructed to take off your shoes and jewelry. You will then be given a sterile hair cap, body garment (you do not take off your clothes) and foot coverings. You will then be led to a preparatory room where an assistant will begin treatment with numbing eye drops.
During Surgery
The surgery should take less than 20 minutes. You will lie on your back in a reclining chair in an exam room containing the laser system. The laser system includes a large machine with a microscope attached to it and a computers screen.
Another numbing drop will be placed in your eye, the area around your eye will be cleaned, and an instrument called a lid speculum will be used to hold your eyelids open. A ring will be placed on your eye and very high pressures will be applied to create suction to the cornea. Your vision will dim while the suction ring is on and you may feel the pressure and experience some discomfort during this part of the procedure. The microkeratome, a cutting instrument, is attached to the suction ring. Your doctor will use the blade of the microkeratome to make a flap in you cornea.
The microkeratome and the suction ring are then removed. You will be able to see, but you will experience fluctuating degrees of blurred vision during the rest of the procedure. The doctor will then lift the flap and fold it back on its hinge, and dry the exposed tissue.
The laser will be positioned over your eye and you will be asked to stare at a light. This is not the laser used to remove tissue from the cornea. This light is to help you keep your eye fixed on one spot once the laser comes on. NOTE: if you cannot stare at a fixed object for at least 60 seconds, you may not be a good candidate for this surgery.
When your eye is in the correct position, your doctor will start the laser. At this point in the surgery, you may become aware of new sounds and smells. The pulse of the laser makes a ticking sound. As the laser removes corneal tissue, some people have reported a smell similar to burning hair. A computer controls the amount of laser energy delivered to your eye. Before the start of surgery, your doctor will have programmed the computer to vaporize a particular amount of tissue based on the measurements taken at your initial evaluation. After the pulses of laser energy remove the exact amount of corneal tissue, your eye is irrigated and then the flap is put back into position.
After Surgery
Immediately after the procedure, your eye may burn, itch, or feel like there is something in it. You may experience some discomfort , or in some cases, mild pain and your doctor may suggest you take a mild pain reliever. Both your eyes may tear or water. Your vision will probably be hazy or blurry. You will instinctively want to rub your eye, BUT DON”T!! Rubbing your eye could dislodge the flap, requiring further treatment. In addition, you may experience sensitivity to light glare, starburst or haloes around lights, or the whites of your eye may look red or bloodshot. These symptoms should improve considerably within the first few days after surgery. You should plan on taking a few days off from work until these symptoms subside. You should contact your doctor immediately and not wait for your scheduled visit, if you experience severe pain, or if your vision or other symptoms get worse instead of better.
You will be given antibiotic eye drops and a lubricating eye drops to use in the weeks following your surgery.
Your doctor will then schedule a follow up visit for the following day to examine you eyes and test your vision. You should have another follow up exam three days after surgery, one month and three months.
If you choose to use your own eye care professional, your doctor will require pre- and post-operative forms. After your 24-hour post-operative appointment you will receive, via email or in person, your refractive surgical report and post-op form for your own eye care doctor.
Day of laser eye surgery (after your surgery)
- The day of surgery should be a day of rest.
- Always be very careful about activities where the eye may be poked, rubbed or touched.
- Always avoid rubbing eyes. Rubbing is never a good idea – instead use lubricating drops for irritation.
- Avoid staring without lubricating the eyes.
24 hours after laser eye surgery.
- Take a bath instead of a shower .Avoid getting soap or water in the eyes.
- Restrict movement to light activities. Work should probably be avoided. Work at home is acceptable.
- Driving short distances after the eye examination is acceptable if adequate vision is confirmed at the post operative evaluation.
- Reading and watching television is acceptable as long as adequate eye lubrication is maintained.
- Flying in airplanes is acceptable but keep eyes generously lubricated (every 30 minutes) airplanes have very dry air.
48 hours after surgery
- Driving can be resumed if adequate vision is confirmed at post-operative evaluation.
- Shower, but continue to avoid any soap or water in the eyes.
- Apply face make-up but not eye make-up.
- Do office work.
- Use computers, but it is very important to keep eyes well lubricated.
Day 3 activities
- Exercise without risk to the eyes, e.g., treadmill, stair climber, stationary bike
- Sexual activity (avoid touching near the eyes)
- Playing with children (be careful)
- Drinking alcohol
Day 7 activities
- Applying eye make-up (avoid touching the eye)
- Jogging outdoors
- Rollerblading
- Relaxed bicycling, no mountain biking
- Playing golf
- Lifting weights
Activities for 1 month after surgery (maintain eye protection for 6 months following any eye surgery)
- Racquet sports – squash, racquetball, badminton (always wear eye protection)
- Swimming
- Scuba diving, snorkeling
- Sailing
- Sun tanning
- Motorcycling, dirt biking, mountain biking
- Parachuting
- Baseball, basketball, football, soccer, hockey
- Skiing
Activities for 3 months after surgery (maintain eye protection for 6 months following surgery)
Proceed with caution as these activities have a high risk of water being forced into the eyes.
- Water skiing
- Wind surfing
- Kayaking
- Surfing
6-. When should You NOT have LASIK
If you have any of the following situations or conditions, the risk of LASIK surgery may be greater than the benefit. You should consider NOT having LASIK surgery if you:
- Are pregnant or nursing. These conditions may cause temporary and unpredictable changes in your cornea that may interfere with the accuracy of the measurement of your cornea before the LASIK procedure.
- Have a collagen vascular (e.g., rheumatoid arthritis), autoimmune (e.g., lupus), or immunodeficiency disease (e.g., AIDS). These conditions affect your body’s ability to heal and may result in inflammation or swelling of parts of the body such as muscles, joints, and blood vessels.
- Show signs of keratoconus
by SSI VA
Categories
Recent Posts
-

Dental Implants
Dec, 30, 2015
-
General Dental Crowns
Dec, 30, 2015
-
Terms & Conditions
May, 26, 2015
-
Payment & Privacy Terms
May, 26, 2015
-
Dental Surgery
May, 26, 2015
-
Orthopedic & General Surgery:
May, 26, 2015
-
Eye Surgery
May, 26, 2015
-
Plastic Surgery:
May, 26, 2015
-
Site Map
May, 26, 2015
-
Links
May, 26, 2015












Leave a Comment